Phimosis

Allo Health is dedicated to personalized well-being, offering support and trusted information tailored to individual health goals. The platform emphasizes human-generated content, led by a distinguished medical team of experts, including physicians and sexual health specialists. Their commitment to credibility involves rigorous fact-checking, authoritative research, and continuous updates to ensure accurate, up-to-date information. Allo Health's unique approach goes beyond conventional platforms, providing expert-led insights and a continuous commitment to excellence, with user feedback playing a crucial role in shaping the platform's authoritative voice.

A Psychotherapist with Clinical specialization, working for over seven years now. Areas of specialization range from Anxiety-related disorders, Mood-related disorders, Personality disorders, Sexual dysfunctions & other mental health issues.
Why This Was Upated?
Our experts continually monitor the health and wellness space, and we update our articles when new information became available.
Updated on 01 June, 2024
- Article was updated as part of our commitment to diversity, equity, and inclusion.

"The following blog article provides general information and insights on various topics. However, it is important to note that the information presented is not intended as professional advice in any specific field or area. The content of this blog is for general educational and informational purposes only.
Book consultation
The content should not be interpreted as endorsement, recommendation, or guarantee of any product, service, or information mentioned. Readers are solely responsible for the decisions and actions they take based on the information provided in this blog. It is essential to exercise individual judgment, critical thinking, and personal responsibility when applying or implementing any information or suggestions discussed in the blog."
What is Phimosis?
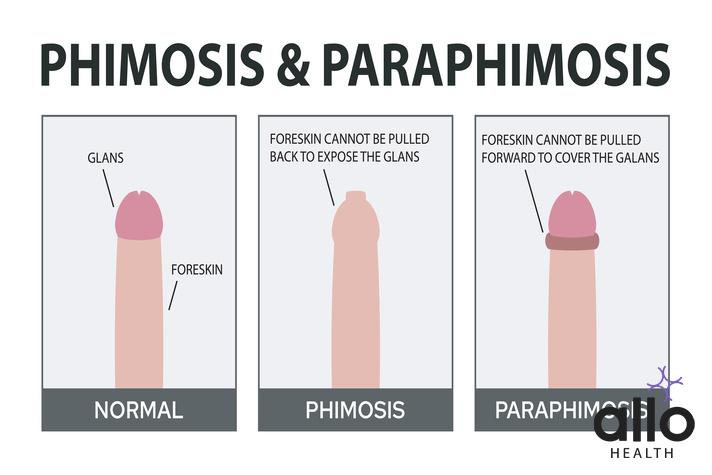
Phimosis is a medical condition that affects males, particularly infants, children, and occasionally adults. It refers to the inability to retract the foreskin (the loose skin covering the head of the penis) fully or partially over the glans (the rounded tip of the penis). This condition can make it challenging to clean the area beneath the foreskin, potentially leading to discomfort, inflammation, and other complications.
Phimosis can be classified into two main types: physiological and pathological.
- Physiological Phimosis: This is a normal condition commonly observed in infants and young boys. The foreskin is usually attached to the glans at birth and gradually separates over time. By the age of three, most boys can retract their foreskin without difficulty. In physiological phimosis, the opening of the foreskin is still narrow, but it tends to improve as the child grows.
- Pathological Phimosis: This type of phimosis is often the result of an underlying condition or an issue that inhibits the natural separation of the foreskin from the glans. It can occur in males of any age, including adolescents and adults. Causes of pathological phimosis may include:
- Scarring: Injuries, infections, or inflammation can cause scarring, which restricts the movement of the foreskin.
- Balanitis: This refers to the inflammation of the glans and foreskin, commonly caused by poor hygiene, infections, or certain medical conditions.
- BXO (Balanitis Xerotica Obliterans): It is a chronic, progressive condition characterized by white patches, scarring, and narrowing of the foreskin opening.
- Infections: Repeated or severe infections in the genital area can lead to inflammation and tightening of the foreskin.
- Trauma: Previous surgeries or injuries to the penis can cause scarring and subsequent phimosis.
Treatment options for phimosis depend on the severity, age of the patient, and associated symptoms. They can be categorized as conservative (non-surgical) or surgical methods:
Conservative Treatment
- Topical Steroid Cream: Corticosteroid creams can be applied to the tight foreskin to reduce inflammation and promote the stretching of the skin.
- Manual Stretching Exercises: Gradual manual retraction of the foreskin, performed under the guidance of a healthcare professional, can help loosen the tight area over time.
- Good Hygiene Practices: Maintaining proper hygiene by gently cleaning the area can help prevent infections and alleviate symptoms.
Surgical Treatment
- Circumcision: This involves the surgical removal of the foreskin. It is usually recommended for persistent or severe cases of phimosis that do not respond to conservative treatments.
- Preputioplasty: This surgical procedure involves making a small incision in the tight foreskin to widen the opening while preserving the foreskin.
Phimosis Types
Phimosis can be categorized into two main types: physiological phimosis and pathological phimosis. Let’s explore each type in detail:
- Physiological Phimosis: Physiological phimosis is a natural condition that is commonly observed in infants and young boys. It occurs due to the normal development of the foreskin and its gradual separation from the glans (the rounded tip of the penis). In this type of phimosis, the foreskin is still attached to the glans but usually becomes more retractable as the child grows older. By the age of three, most boys can fully retract their foreskin without any difficulty or discomfort.
Physiological phimosis is considered a normal variant of penile development and does not typically require medical intervention. As the child matures, the foreskin gradually separates, and the opening widens, allowing for easier retraction.
- Pathological Phimosis: Pathological phimosis refers to the condition where the foreskin cannot be fully or partially retracted due to an underlying issue or an abnormality. This type of phimosis can affect males of any age, including adolescents and adults. Pathological phimosis can be caused by various factors, including:
- Scarring: Scarring of the foreskin or the glans can occur as a result of previous injuries, infections, or inflammation. The scar tissue can lead to a narrowing or tightening of the foreskin, making it difficult to retract.
- Balanitis: Balanitis is the inflammation of the glans and foreskin, which can be caused by poor hygiene, infections, or certain medical conditions. Inflammation and swelling can lead to the tightening of the foreskin.
- BXO (Balanitis Xerotica Obliterans): BXO is a chronic, progressive condition characterized by white patches, scarring, and fibrosis of the foreskin and glans. It can cause significant narrowing of the foreskin opening, leading to phimosis.
- Infections: Repeated or severe infections in the genital area, such as recurrent balanitis or sexually transmitted infections, can cause inflammation and scarring, resulting in phimosis.
- Trauma: Previous surgeries, injuries, or trauma to the penis can cause scarring and subsequent phimosis.
Pathological phimosis may cause symptoms such as pain, discomfort, difficulty urinating, ballooning of the foreskin during urination, recurrent infections, or hygiene-related concerns. Treatment options for pathological phimosis include conservative (non-surgical) methods and surgical interventions, as mentioned in the previous response.
Is Phimosis Common In India: Incidence & Prevalence
Phimosis is relatively common in India, with a higher prevalence compared to some other countries. The exact incidence and prevalence rates can vary depending on the population studied and the methodology used to determine the prevalence. However, several studies have provided insights into the occurrence of phimosis in India.
- Pediatric Phimosis: Pediatric phimosis refers to the condition observed in infants and children. It is considered a normal developmental phase in most cases, and the majority of children naturally outgrow it as they get older. However, in some cases, pathological phimosis may persist or develop.
- Incidence: The incidence of pediatric phimosis in India varies across studies. A study published in the Indian Journal of Urology reported an incidence of 91.6% among children aged 0-10 years who visited a pediatric surgery outpatient department. Another study published in the Journal of Indian Association of Pediatric Surgeons reported an incidence of 15.4% among boys aged 6 months to 11 years.
- Prevalence: The prevalence of pediatric phimosis in India is relatively high. A study published in the Indian Journal of Urology reported a prevalence rate of 17.1% among boys aged 0-10 years. Another study published in the Journal of Pediatric Urology reported a prevalence rate of 13.7% among boys aged 5-10 years.
- Adult Phimosis: Adult phimosis refers to the condition that persists or develops in males beyond childhood.
- Prevalence: The prevalence of adult phimosis in India is relatively high compared to some other countries. A study published in the Indian Journal of Dermatology reported a prevalence rate of 21.7% among males aged 18-60 years attending a dermatology outpatient department. Another study published in the Indian Journal of Urology reported a prevalence rate of 2.9% among adult males attending a urology outpatient department.
Diagnosis
The diagnosis of phimosis involves a comprehensive evaluation by a healthcare professional, typically a urologist or pediatrician. The healthcare provider will gather information about the patient’s medical history, perform a physical examination, and may order additional tests if necessary. Here is a detailed overview of the diagnosis process for phimosis:
- Medical History: The healthcare provider will begin by asking questions about the patient’s medical history, including:
- Symptoms: The patient will be asked about any symptoms they are experiencing, such as pain, discomfort, difficulty urinating, recurrent infections, or hygiene-related concerns.
- Age of Onset: The healthcare provider will inquire about when the symptoms or concerns regarding the foreskin’s tightness or inability to retract were first noticed.
- Previous Injuries or Surgeries: Any history of injuries, surgeries, or trauma to the genital area will be discussed.
- Infections: The healthcare provider may ask about any previous or current infections in the genital region, including balanitis or sexually transmitted infections.
- Hygiene Practices: The patient’s hygiene practices, including how they clean the genital area, will be evaluated.
- Physical Examination: The healthcare provider will conduct a physical examination of the genital area to assess the condition of the foreskin and the glans. The examination may involve the following:
- Visual Inspection: The healthcare provider will visually inspect the penis and examine the foreskin’s appearance, noting any signs of inflammation, scarring, or infections.
- Foreskin Retraction: They will attempt to retract the foreskin gently to determine the degree of mobility and assess the tightness or constriction. This will be done with caution to avoid causing pain or injury.
- Examination of the Glans: The glans will be examined for any abnormalities, such as signs of infection, scarring, or white patches (which may indicate BXO).
- Additional Tests: In most cases, the diagnosis of phimosis can be made based on the medical history and physical examination. However, additional tests may be recommended in certain situations to assess the severity of the condition or identify any underlying causes. These tests may include:
- Urine Analysis: If there are symptoms of urinary difficulties or recurrent infections, a urine analysis may be performed to check for signs of infection or other abnormalities.
- Biopsy: In cases where there are suspicious lesions or white patches on the foreskin or glans, a biopsy may be performed to confirm the diagnosis of BXO or rule out other potential conditions.
Symptoms
Phimosis can present with various symptoms depending on the severity of the condition and the presence of any associated complications. Here are the symptoms that may be experienced by individuals with phimosis:
- Difficulty or Inability to Retract the Foreskin: The primary symptom of phimosis is the inability to retract the foreskin fully or partially over the glans (the rounded tip of the penis). In physiological phimosis (common in infants and young boys), the inability to retract the foreskin is typically temporary and improves as the child grows older. In pathological phimosis, the foreskin remains tight and may cause persistent difficulty or inability to retract.
- Pain or Discomfort: Attempting to retract a tight foreskin can cause pain or discomfort. This can be particularly pronounced during sexual activities or when cleaning the genital area. In some cases, pain may also be experienced during urination if the foreskin restricts the flow of urine.
- Ballooning of the Foreskin: During urination, the urine may accumulate under the foreskin, causing it to balloon or inflate. This happens when the tight opening of the foreskin prevents the urine from freely exiting the penis. Ballooning may be a sign of phimosis and can lead to hygiene difficulties and an increased risk of infections.
- Recurrent Infections: Phimosis can contribute to a higher risk of infections in the genital area. The trapped urine, smegma (a substance that accumulates under the foreskin), and difficulty in proper cleaning can create an environment favorable for the growth of bacteria, leading to recurrent balanitis (inflammation of the glans and foreskin) or other genital infections.
- Redness, Swelling, or Irritation: The restricted foreskin can cause inflammation, redness, swelling, or irritation of the glans and foreskin. These symptoms may be more pronounced during or after sexual activity, urination, or if an infection is present.
Causes Of Phimosis In Adults
Phimosis in adults can occur due to various causes. Unlike in children, where physiological phimosis is common and often resolves naturally, adult phimosis is more likely to be caused by pathological factors. Here are the main causes of phimosis in adults:
- Scarring and Adhesions: Scarring of the foreskin or the glans can result from previous injuries, infections, or inflammation. Scarring can cause the foreskin to become tight and constricted, leading to phimosis. Adhesions, where the inner layer of the foreskin sticks to the glans, can also contribute to the narrowing of the foreskin opening.
- Balanitis Xerotica Obliterans (BXO): BXO is a chronic, progressive condition characterized by white patches, scarring, and fibrosis of the foreskin and glans. The exact cause of BXO is unknown, but it is believed to involve an autoimmune or inflammatory response. BXO can lead to significant narrowing and constriction of the foreskin, resulting in phimosis.
- Infections: Infections in the genital area can contribute to the development of phimosis in adults. Recurrent or severe infections, such as balanitis (inflammation of the glans and foreskin) or sexually transmitted infections, can cause inflammation, scarring, and tightening of the foreskin.
- Diabetes: Uncontrolled or poorly managed diabetes can lead to an increased risk of developing phimosis. Elevated blood sugar levels can impair the body’s ability to fight infections and heal wounds, making individuals with diabetes more susceptible to foreskin inflammation, scarring, and subsequent phimosis.
- Trauma or Injuries: Previous surgeries, injuries, or trauma to the penis can cause scarring, adhesions, or structural changes in the foreskin, leading to phimosis. Trauma may occur due to accidents, aggressive sexual practices, or medical procedures involving the genital area.
- Other Medical Conditions: Certain medical conditions may predispose individuals to phimosis. For example, lichen sclerosus is a chronic inflammatory condition that can affect the genital skin, causing thinning, scarring, and phimosis. Other skin disorders, such as psoriasis or eczema, can also contribute to the development of phimosis.
Risk Factors
Several factors can increase the risk of developing phimosis. While some risk factors are specific to certain age groups, others can apply to individuals of all ages. Here are the main risk factors associated with phimosis:
- Age: Phimosis is more common in certain age groups. Physiological phimosis, which is the normal developmental phase in infants and young boys, is most prevalent in this age range. Pathological phimosis, on the other hand, can occur at any age, including adolescence and adulthood.
- Poor Hygiene: Inadequate or improper genital hygiene practices can contribute to the development of phimosis. If the area beneath the foreskin is not cleaned regularly and thoroughly, smegma (a substance comprising dead skin cells, oils, and other bodily fluids) can accumulate, leading to inflammation, infections, and scarring.
- Infections: Repeated or severe infections in the genital area, such as balanitis (inflammation of the glans and foreskin), can cause scarring and subsequent phimosis. Infections can result from poor hygiene, sexually transmitted infections, or other factors that compromise the immune system’s ability to fight off infections.
- Preputial Ballooning: Preputial ballooning refers to the trapping of urine beneath the foreskin during urination due to a tight foreskin opening. This condition can stretch the foreskin and contribute to the development of phimosis.
- Diabetes: Individuals with diabetes, especially when the condition is poorly controlled, may be at an increased risk of developing phimosis. Elevated blood sugar levels can impair the body’s ability to fight infections and heal wounds, making the foreskin more susceptible to inflammation, scarring, and subsequent phimosis.
- Trauma or Injuries: Previous surgeries, injuries, or trauma to the penis can lead to scarring, adhesions, or structural changes in the foreskin, increasing the risk of phimosis. Trauma may result from accidents, aggressive sexual practices, or medical procedures involving the genital area.
- Certain Medical Conditions: Certain medical conditions, such as lichen sclerosus (a chronic inflammatory condition affecting the genital skin), psoriasis, or eczema, can predispose individuals to phimosis. These conditions can cause skin changes, scarring, and tightening of the foreskin.
Treatment Of Phimosis
The treatment of phimosis depends on several factors, including the age of the individual, the severity of the condition, the presence of symptoms, and the underlying cause. Treatment options can range from conservative (non-surgical) methods to surgical interventions. Here are the main treatment approaches for phimosis:
- Conservative Treatment:
- Topical Steroid Cream: Corticosteroid creams or ointments can be prescribed to apply to the tight foreskin. These creams help reduce inflammation and promote the stretching and loosening of the skin. The cream is typically applied to the narrowed area of the foreskin, and gentle manual retraction may be performed under the guidance of a healthcare professional. This approach is most effective in cases of physiological phimosis or mild pathological phimosis.
- Manual Stretching Exercises: Under the guidance of a healthcare professional, manual stretching exercises can be performed to gradually loosen the foreskin. This involves gently retracting the foreskin on a regular basis to stretch the opening. This approach is usually recommended for mild to moderate cases of phimosis.
- Good Hygiene Practices:
- Maintaining proper hygiene is essential to prevent infections and alleviate symptoms. Regular and thorough cleaning of the genital area is important, paying attention to gently retract the foreskin and clean beneath it. Warm water and mild soap can be used for cleaning, and it is important to avoid harsh soaps or irritants that can cause further inflammation.
- Surgical Treatment:
- Circumcision: Circumcision is the surgical removal of the foreskin. It is the most common surgical treatment for phimosis, particularly in cases where conservative methods have failed or when the phimosis is severe, persistent, or causing significant symptoms. Circumcision involves the complete removal of the foreskin, exposing the glans. It is a permanent solution to phimosis but requires a surgical procedure and recovery period.
- Preputioplasty: Preputioplasty is a surgical procedure aimed at widening the opening of the foreskin without removing it entirely. It involves making a small incision in the narrowed area and then suturing the incision in a way that allows for a wider opening. Preputioplasty preserves the foreskin while addressing the tightness. It is an alternative to circumcision in cases where preserving the foreskin is desired.
The choice of treatment depends on the individual’s circumstances and preferences, as well as the healthcare professional’s assessment. It is important to consult with a healthcare professional, such as a urologist or pediatrician, for an accurate diagnosis and appropriate treatment plan for phimosis. They can evaluate the specific case, discuss the pros and cons of each treatment option, and recommend the most suitable approach.
Prevention
While some cases of phimosis are physiological and part of normal development in infants and young boys, there are preventive measures that can help reduce the risk or severity of pathological phimosis. Here are some key prevention strategies for phimosis:
- Proper Hygiene Practices:
- Regular Cleaning: Teach boys and men proper hygiene practices to ensure regular cleaning of the genital area, including under the foreskin. Gently retracting the foreskin and cleaning beneath it during bathing can help prevent the accumulation of smegma (a substance comprising dead skin cells, oils, and bodily fluids) and reduce the risk of inflammation and infections.
- Avoid Trauma or Injury:
- Protective Measures: Encourage individuals to take precautions to prevent injuries or trauma to the genital area. This includes wearing appropriate protective gear during sports activities or engaging in sexual practices that minimize the risk of injury.
- Prompt Treatment of Infections:
- Timely Medical Attention: Infections in the genital area, such as balanitis or sexually transmitted infections, should be promptly diagnosed and treated to prevent complications and reduce the risk of scarring or inflammation that could lead to phimosis.
- Diabetes Management:
- Effective Diabetes Control: Individuals with diabetes should strive to maintain optimal blood sugar control through lifestyle modifications, medication adherence, and regular medical follow-up. Proper diabetes management can help reduce the risk of complications, including infections and potential contributions to phimosis.
- Seek Medical Evaluation:
- Early Diagnosis and Treatment: If there are any concerns or symptoms related to the tightness of the foreskin, it is important to seek medical evaluation. Early diagnosis and appropriate treatment can prevent the progression of phimosis and minimize complications.
Uncircumcised Penis and Phimosis: Is There A Correlation?
There is a correlation between having an uncircumcised penis and the development of phimosis. Phimosis refers to the inability to fully or partially retract the foreskin over the glans (the rounded tip of the penis). Uncircumcised individuals have a foreskin that naturally covers and protects the glans, and in some cases, this foreskin may become tight or narrow, leading to phimosis.
Here’s how the correlation between an uncircumcised penis and phimosis can be explained:
- Physiology: In infants and young boys, the foreskin is typically attached to the glans at birth. Over time, it gradually separates, allowing for the natural retraction of the foreskin. However, in some individuals, the separation process may be slower, leading to a naturally tighter or narrower foreskin, known as physiological phimosis. This condition is common in infants and young boys and tends to improve as they grow older.
- Hygiene and Infections: The accumulation of smegma, a substance comprising dead skin cells, oils, and bodily fluids, can occur under the foreskin if proper hygiene is not maintained. Insufficient cleaning of the genital area can lead to irritation, inflammation, and infections, which can contribute to the development of phimosis.
- Ballooning: During urination, the urine may become trapped under the tight foreskin, causing it to balloon or inflate. This condition, known as preputial ballooning, is more likely to occur in individuals with a tight foreskin. Ballooning can lead to further hygiene difficulties and an increased risk of infections.
Frequently Asked Questions
- Is phimosis common?
Phimosis is relatively common, particularly in infants and young boys. While physiological phimosis is normal and tends to resolve naturally as children grow older, pathological phimosis can occur in individuals of any age, including adults. - Can phimosis resolve on its own?
Physiological phimosis in infants often resolves spontaneously as part of normal development. However, pathological phimosis may require treatment as it usually does not resolve on its own. - How is phimosis diagnosed?
Diagnosis of phimosis involves a medical history assessment and a physical examination of the genital area. The healthcare provider may attempt to gently retract the foreskin to evaluate its mobility and assess the severity of the condition. In some cases, additional tests may be conducted to determine the underlying cause. - Can phimosis be prevented?
While phimosis cannot always be prevented, practicing good hygiene by regularly cleaning the genital area and promptly treating infections or inflammations can help reduce the risk of developing phimosis. - What are the treatment options for phimosis?
Treatment options for phimosis include conservative approaches and surgical interventions. Conservative methods include the use of topical steroid creams to reduce inflammation and promote stretching, as well as manual stretching exercises. Surgical options include circumcision, the removal of the foreskin, or preputioplasty, a procedure that widens the foreskin opening while preserving the foreskin. - How effective are steroid creams for phimosis?
Topical steroid creams have shown effectiveness in reducing inflammation and facilitating foreskin stretching in mild cases of phimosis. However, their success may vary depending on the individual and the severity of the condition. - Is surgery always necessary for phimosis?
Surgery is not always necessary for phimosis. Conservative methods are usually attempted first, especially in mild cases or in children. Surgery is considered if conservative approaches fail or if the phimosis is severe, persistent, or causing significant symptoms. - Is circumcision the only surgical option for phimosis?
No, circumcision is not the only surgical option. Preputioplasty is an alternative procedure that aims to widen the foreskin opening while preserving the foreskin itself. It may be recommended in cases where preserving the foreskin is desired. - Are there any risks or complications associated with phimosis treatment?
While the risks are generally low, surgical interventions for phimosis may carry potential complications such as bleeding, infection, or scarring. Conservative treatments typically have minimal risks. - Can adults develop phimosis even if they were not previously affected?
Yes, adults can develop phimosis even if they did not experience it during childhood. Factors such as infections, scarring from trauma, or certain medical conditions can lead to the development of phimosis in adulthood. - Does phimosis affect sexual function?
Phimosis can occasionally cause discomfort or pain during sexual activity. However, treating phimosis can alleviate such concerns and improve sexual comfort and function. - Can phimosis lead to other complications?
Phimosis can lead to complications such as recurrent infections, inflammation, difficulty urinating, and potential impact on overall genital health. Timely treatment is essential to prevent such complications and maintain proper genital hygiene and function.











































